Life Threatening Link Diabetes And Clots
Imagine waking up with a tight, painful calf after a long weekend of gardening. You shrug it off, but the pain worsens and your leg swells. Could it be a simple muscle strain — or something much more serious? For people with diabetes, that nagging question touches on a very real concern: the life threatening link diabetes and clots. Understanding this connection can save limbs and lives.
Why diabetes raises your risk of dangerous blood clots
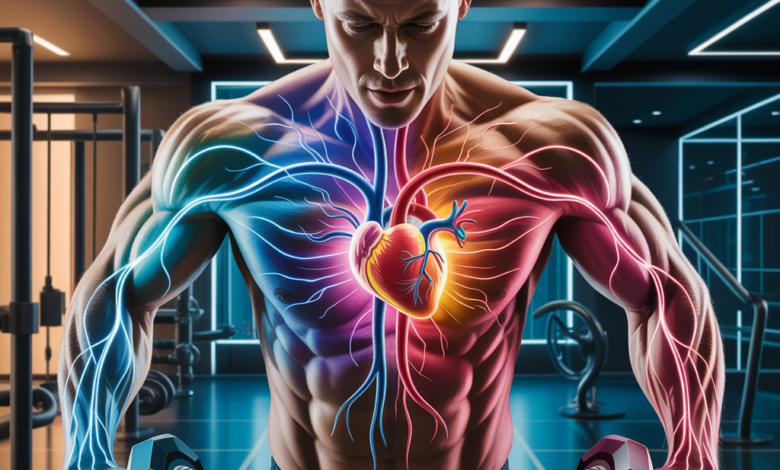
Diabetes doesn’t just affect blood sugar. Chronic high glucose levels lead to inflammation, damage to blood vessel linings (endothelial dysfunction), and altered platelet activity — all of which increase the chance of thrombosis (blood clot formation). Both arterial clots (which can cause heart attacks and strokes) and venous clots (like deep vein thrombosis or pulmonary embolism) are more common in people with type 1 and type 2 diabetes.
The biological picture in plain English
- High blood sugar irritates vessel walls, making them sticky and inflamed.
- Platelets become more reactive, so clots form faster and are harder to break down.
- Diabetes is often accompanied by obesity, high blood pressure, and high cholesterol — additional clotting risk factors.
Signs and symptoms to take seriously
Recognizing symptoms early can make the difference between a minor medical visit and an emergency. Watch for:
- Unilateral leg swelling, warmth, redness, or severe calf pain (possible DVT)
- Sudden chest pain, shortness of breath, or coughing up blood (possible pulmonary embolism)
- Sudden numbness, slurred speech, or facial droop (possible stroke)
- Unexplained limb pain, coldness, or pale skin (possible arterial clot)
If you have diabetes and experience any of these, seek immediate medical attention.
Practical lifestyle strategies to reduce clot risk
While medication and regular medical follow-up are essential, everyday habits play a powerful role in lowering clot risk. These are realistic, science-backed changes you can start this week.
Move more — and move smart
- Daily walks: Aim for 30 minutes most days. Walking improves circulation and insulin sensitivity.
- Break up sedentary time: Stand or walk for a few minutes every hour, especially if you work at a desk or travel often.
- Leg-focused exercises: Calf raises, hamstring curls, and seated marches stimulate venous return and reduce pooling.
- HIIT and strength training: Two sessions per week of resistance training plus one HIIT session can improve vascular health and body composition.
Try a simple routine: 5-minute warm-up walk, 3 sets of 12 squats or chair squats, 3 sets of 15 calf raises, then a 10-minute brisk walk or interval sprints. Bookmark our workout routines for more variations and beginner-friendly plans.
Eat with circulation and inflammation in mind
- Focus on anti-inflammatory foods: leafy greens, berries, fatty fish rich in omega-3s, nuts, and olive oil.
- Limit refined carbs and added sugars: these spike blood glucose and fuel inflammation that promotes clotting.
- Prioritize fiber and lean protein: they stabilize blood sugar and support overall vascular health.
- Stay hydrated: dehydration thickens blood and can increase clot risk.
If you want meal ideas that support vascular health and blood sugar balance, check our nutrition guides.
Fitness tips for people with diabetes: safety and variety
Exercise is one of the best defenses against the life threatening link diabetes and clots, but safety matters. Follow these practical tips to stay active while managing diabetes.
Warm-up and cool down
- Always start with 5–10 minutes of gentle movement to increase blood flow and reduce injury risk.
- Finish with stretching and light activity to prevent blood pooling in the legs.
Adjust workouts based on blood sugar
- Monitor glucose before and after exercise if you’re on insulin or blood sugar–lowering medications.
- Keep a fast-acting carb (juice or glucose tablets) available in case of hypoglycemia during longer workouts.
Low-impact options that protect joints and boost circulation
- Swimming or water aerobics — excellent for people with neuropathy or joint pain.
- Cycling — improves leg circulation without high-impact stress.
- Yoga and Pilates — encourage mobility, balance, and stress reduction, which indirectly support vascular health.
Real-world example: Maria, 58, diagnosed with type 2 diabetes, swapped two weekly long runs for a mix of brisk walking, resistance bands, and pool sessions after a DVT scare. Her circulation improved, her meds were reviewed, and she lowered her HbA1c — small shifts that added up to big risk reduction.
Medical management and when to consult your doctor
Preventing clots in people with diabetes may include medication, especially if you have additional risk factors like recent surgery, a history of clots, or prolonged immobility. Your clinician may talk about anticoagulants, antiplatelet therapy, or optimizing glucose, blood pressure, and cholesterol control.
Regular check-ups, foot exams, and vascular screenings are vital. Discuss personal risk with your healthcare provider — personalized plans beat generic advice every time. For everyday wellness tips that support medical care, visit our wellness tips page.
Frequently Asked Questions
Q: Can diabetes directly cause blood clots?
A: Diabetes creates an environment — inflammation, endothelial damage, and platelet hyperactivity — that increases the likelihood of clot formation. It’s a contributing factor rather than a single direct cause, and risks grow when combined with obesity, smoking, high blood pressure, or prolonged immobility.
Q: What exercises help prevent clots for people with diabetes?
A: Regular walking, calf-strengthening moves, cycling, swimming, and strength training all promote circulation and reduce clot risk. Breaking up long periods of sitting with short walks is one of the simplest, most effective habits.
Q: Are there foods that reduce the risk of clots?
A: A Mediterranean-style diet rich in omega-3s (fatty fish), antioxidants (berries, leafy greens), whole grains, and healthy fats (olive oil, nuts) helps lower inflammation and supports vascular health. Avoiding excess sugar and refined carbs is equally important.
Conclusion — take action today
The life threatening link diabetes and clots is real, but it’s manageable. By combining smart exercise, anti-inflammatory nutrition, hydration, and regular medical care, you dramatically reduce your risk. Start with small, consistent steps: a daily 30-minute walk, two resistance sessions a week, and a weekly check of your blood sugar and shoes. If you’re concerned about clot risk or have symptoms, contact your healthcare provider immediately.
Ready to get started? Explore tailored workout routines, practical nutrition guides, and more wellness tips to protect your vascular health. Don’t wait — your circulation, mobility, and peace of mind are worth the effort.





